Not known Facts About Medigap Cost Comparison Chart
Wiki Article
The Only Guide to Medicare Part C Eligibility
Table of Contents6 Easy Facts About Boomer Benefits Reviews DescribedThe smart Trick of Medicare Supplement Plans Comparison Chart 2021 Pdf That Nobody is Talking AboutThe 15-Second Trick For Medicare Supplement Plans Comparison Chart 2021 PdfNot known Details About Apply For Medicare Medigap Cost Comparison Chart for BeginnersThe 5-Minute Rule for Shingles Vaccine Cost
Nelson does not need to file an application for Premium-Part A since he lives in a Component A Buy-in State. The FO refers Mr. Nelson to his State to apply for the QMB Program, according to instructions in HI 00801. 140E.3 of this area. (Note: If Maryland approves Mr. Nelson's application for the QMB Program, the State will certainly enlist him in State Buy-in due to the fact that he already has Component B.
Review listed below to locate out-- If he has Medicaid or QMB, just how a lot will Medicaid pay?!? SHORT RESPONSE: QMB or Medicaid will pay the Medicare coinsurance only in restricted scenarios.

A Biased View of Apply For Medicare
This creates stress in between a private as well as her doctors, drug stores giving Part B medicines, and also other suppliers. Providers might not know they are not allowed to bill a QMB recipient for Medicare coinsurance, considering that they bill other Medicare beneficiaries. Also those who know may push their individuals to pay, or merely decrease to offer them.2 (who can help me choose a medicare plan). Exactly how Does a Supplier that DOES accept Medicaid Costs for a QMB Beneficiary? The supplier expenses Medicaid - even if the QMB Recipient does not likewise have Medicaid. Medicaid is required to pay the carrier for all Medicare Part An and also B cost-sharing costs for a QMB recipient, even if the solution is normally not covered by Medicaid (ie, chiropractic, podiatry as well as professional community service care).
Cuomo has actually recommended to lower how much Medicaid pays for the Medicare costs even additionally (shingles vaccine cost). The quantity Medicaid pays is various relying on whether the individual has Original Medicare or is a Medicare Advantage strategy, with much better repayment for those in Medicare Benefit strategies. The solution also differs based upon the type of service.
Aarp Plan G Fundamentals Explained
- - Presently, Medicaid pays the full Medicare accepted fees until the beneficiary has satisfied the annual insurance deductible, which is $198 in 2020. Dr. John charges $500 for a check out, for which the Medicare accepted cost is $198. Medicaid pays the whole $198, fulfilling the insurance deductible. If the recipient has a spend-down, then the Medicaid repayment would be subject to the spend-down.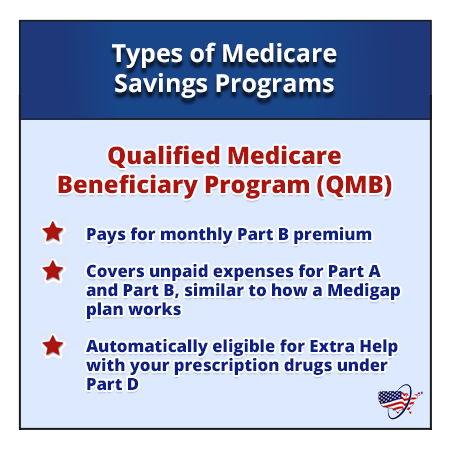
If the Medicaid price for the very same service is just $80 or much less, Medicaid would pay nothing, as it would certainly consider the doctor totally paid = the company has received the full Medicaid rate, which is lesser than the Medicare rate. s - Medicaid/QMB wil pay the full coinsurance for the adhering to solutions, no matter the Medicaid price: ambulance as well as psychologists - The Gov's 2019 proposition to remove these exceptions was declined.
A Biased View of Medicare Select Plans
50 of the $185 accepted rate, provider will ideally not be deterred from offering Mary or other QMBs/Medicaid receivers. - The 20% coinsurance is $37. Medicaid pays none of the coinsurance because the Medicaid price ($120) is lower than the amount the provider already gotten from Medicare ($148). For both Medicare Advantage and Original Medicare, if the costs was for a, Medicaid would pay the complete 20% coinsurance despite the Medicaid rate.If the carrier desires Medicaid to pay the coinsurance, then the supplier must register as a Medicaid provider under the state guidelines. This is a modification in policy in applying Area 1902(n)( 3 )(B) of the Social Security Act (the Act), as changed by area 4714 of the Well Balanced Spending Plan Act of 1997, which prohibits Medicare suppliers from balance-billing QMBs for Medicare cost-sharing.
This area of the Act is readily available at: CMCS Educational Notice . QMBs have no lawful responsibility to make further payment to a company or Medicare handled care prepare for Part A or Part B expense sharing. Providers who inappropriately bill QMBs for Medicare cost-sharing undergo assents. Please keep in mind that the statute referenced above supersedes CMS State Medicaid Handbook, Chapter 3, Qualification, 3490.
The 30-Second Trick For Apply For Medicare
See this passage of the 2017 call letter by Justice in Aging - It can be tough to reveal a carrier that one is a QMB. It is particularly hard for companies that are not Medicaid providers to recognize QMB's, considering that they do not have accessibility to on the internet Medicaid qualification systems If a consumer reports a balance billng trouble to this number, the Consumer Service Representative can escalate the problem to the Medicare Administrative Contractor (MAC), which will certainly send a compliance letter to the carrier with a copy to the consumer.50 of the $185 accepted rate, supplier will hopefully not be discouraged from serving Mary or other QMBs/Medicaid recipients. - The 20% coinsurance is $37. Medicaid pays none of the coinsurance since the Medicaid rate ($120) is less than the quantity the provider currently gotten from Medicare ($148). For both Medicare Advantage and also Original Medicare, if the costs was for a, Medicaid would pay the full 20% coinsurance despite the Medicaid price.
If the company wants Medicaid to pay the coinsurance, after that the service provider should sign up as a Medicaid supplier under the state guidelines. This is a change in plan in implementing Area 1902(n)( 3 )(B) of the Social Safety And Security Act (the Act), as modified by area 4714 of the Well Balanced Spending Plan Act of 1997, which bans Medicare suppliers from balance-billing QMBs for Medicare cost-sharing.
Indicators on Aarp Plan G You Should Know
This section of the Act is available at: CMCS Informational Publication . QMBs have no lawful obligation to make further repayment to a carrier or Medicare took care of treatment strategy for Part A or Part B cost sharing. Companies who inappropriately bill QMBs for Medicare cost-sharing are subject to sanctions. Please note that the law referenced above supersedes CMS State Medicaid Manual, Phase 3, Qualification, 3490.
Report this wiki page